Maternal positioning: what the heck does that mean? Well, let’s break it down…
Maternal – mother
Positioning – arrangement of the mother’s body as it pertains to labour
Anecdotally, it is believed that the position of a pregnant person can play a significant role in changing baby’s position from occiput posterior (OP) to occiput anterior (OA) during labour (See Figure 1). An OP position often can cause anxiety for the mother because it has been proven true with research that an OP position can possibly lead to a more difficult labour in terms of being slow to start, more pain in the back or “back labour”, and an increased risk of medical interventions such as forceps, vacuum, or cesarean delivery. That being said, an OP positioned baby does not have to mean a worse birthing experience. There is currently no science to support the theory that the birthing person has control over whether baby will be delivered as OP or OA.
As babies are coming down the birth canal and through the pelvis, they typically rotate. The reason for this is because the shape of the top of the pelvis is different than its bottom, so babies have to turn to get through each. Because of this rotation, babies will/can enter both an anterior and a posterior position at some point during labour.
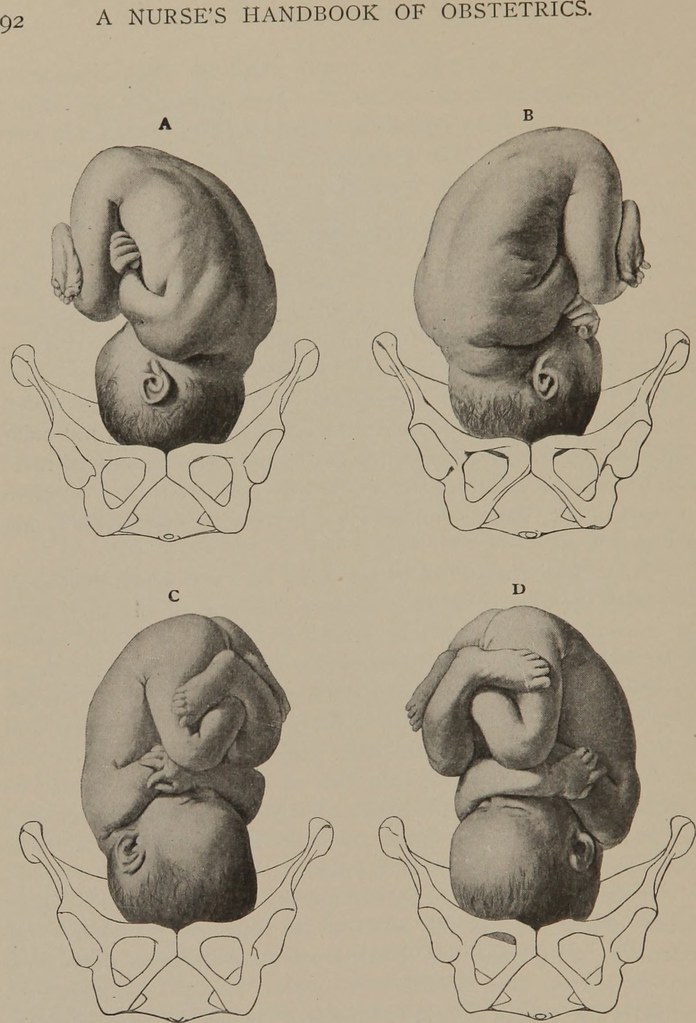
Figure 1. Occiput Anterior (A and B), and Occiput Posterior (C and D).
Whether they end up as anterior or posterior is entirely up to the shape of the baby and the shape of the birthing person’s pelvis, but 5-8% of all births will remain in an OP position into the third stage of labour. The two main reasons that care providers will encourage the birthing person to switch positions during labour are 1) comfort, and 2) rest.
- Comfort. Yes, labour does mean pain. The level of pain and how well the birthing person is coping with this pain varies significantly from person to person, so finding a comfortable position to labour in is key. If a certain position is no longer comfortable, or the birthing person is no longer able to cope with the pain, the care provider, the nurse, the support person, or the doula may suggest switching to another position. Depending on the stage of labour, the birthing person may walk, squat, lean on a birth ball, dance with their support person, take a shower, lay in bed, any/all of the above to seek comfort. In fact, the American College of Obstetricians and Gynecologists found that upright positions, such as walking, kneeling, or standing, as opposed to recumbent or supine positions shortened the length of the first stage of labour by 1 hour and 22 minutes. So, if you are able to, why not try any of the upright positions while in labour – it could make you more comfortable, and it could shorten your first stage of labour!
- Rest. Okay, so rest takes on a different meaning during labour. Rest may not mean a full-on half an hour, REM cycle nap; it may not even mean full rejuvenation or relaxation. Rest during labour might be an epidural after a 36 hour labour. Rest during labour might be a position that alleviates some of gravity’s toll with one leg and upper body resting on the bed. Rest during labour might be a soak in the jet tub in a sitting position. Rest during labour might be manipulating an exercise ball or peanut ball into a restful position. Unfortunately, we as doulas cannot make labour pain any better; neither the ball, the bath, or the bed is better than the other. What we can help you with is to find a position that can possibly give you more comfort, and perhaps some moments of rest.
Although there is no research supporting the theory that maternal positioning can play a role in changing baby’s OP position to a more desirable OA position, what studies do support is that switching positions can have an effect on maternal comfort and rest. Keep in mind, a baby that is in an OP position in late pregnancy does not necessarily mean that baby will be in the same position at delivery, so you might as well try to get some rest while you can!
View comments
+ Leave a comment